Peyronie’s disease (PD) is a curvature of the penis that is sometimes painful and can interfere with sexual function. It is an acquired condition of abnormal fibrous tissue overgrowth of one of the inner layers enveloping of the body of the penis. In other words, the covering of the elastic dual chambers that make up the structural integrity of the penile shaft is scarred.
PD is associated with trauma, and occasionally, from unknown causes. PD scars are associated with over-secretion of collagen due to excessive conversions associated with tissue repair. The signals to limit these scar-forming cells are lost in PD. The resulting abnormal scar affects the elasticity of part of the skin, which fails to expand normally resulting in deviation and curvature. The results can be disfiguring, and have profound adverse effects on sexual functioning, leading to anxiety and depression. Although not often discussed, this condition affects millions of American men.
There is a variety of treatments including pills, creams and penile injections, but very few remedies have been shown to be statistically effective. Double blind studies on intralesional verapamil and interferon have failed to demonstrate any significant differences/improvements in penile deformity, pain, plaque softening or sexual function, and intralesional steroids have not shown objective therapeutic benefit.
Intralesional collagenase clostridium histolyticum (Xiaflex®) injections are the first FDA-approved treatment for PD, and studies demonstrate efficacy, but there have been documented cases of corporal rupture and penile hematoma, and significant penile pain.
Surgical repair has been around for decades, but is associated with penile scarring, shortening of the penis, and erectile dysfunction (ED). There has been recent anecdotal interest in biologic therapies including the use of anti-inflammatory platelet rich plasma (PRP) to treat Peyronie’s disease, but there is still insufficient outcome data.
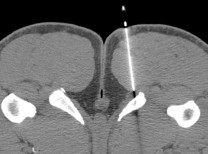
The case is different for stem cell-based research therapy, which may offer a glimpse of hope. The Cell Surgical Network® has been pursuing a cell-based repair for PD as part of an approved investigational program. We are finding that a stem cell-based therapy may mitigate the abnormal cell signals that create excessive scar tissue. The procedure involves isolating autologous (from your own body) stromal vascular fraction (SVF) from 50 cc of adipose tissue aspirated in a sterile, closed system during a two-hour process. Stromal vascular fraction (SVF) is isolated from connective tissues, is associated with subcutaneous fat and blood vessels, and is known to contain adult mesenchymal stem cells and numerous cytokine growth factors.
A Cell Surgical Network® manuscript demonstrating greater than 90% efficacy in treating PD with SVF combined with shock wave therapy has just been accepted for publication by the Plastic and Reconstructive Surgery Global. Some patients required additional treatments to achieve best results. This is the first publication in history showing effectiveness of using stem cells for Peyronie’s disease, and hopefully the beginning of a modern solution to this problem.
Elliot B. Lander, MD, FACS, is co-founder and medical director of The Cell Surgical Network® and medical director of the California Stem Cell Treatment Center in Rancho Mirage and Beverly Hills. He can be reached at (800) 231.0407.


























Comments (0)