This is the latest story in our series about the uses of fat-derived stem cells for the treatment of degenerative diseases.
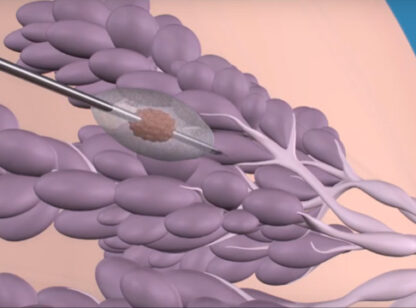
Stem cells can be derived from your own fat as part of a minor outpatient procedure performed as a type of “mini liposuction” under local anesthesia. The product obtained known as Stromal Vascular Fraction (SVF) contains several types of stem cells along with signaling molecules that decrease inflammation and signal the damaged cells to help them heal. SVF can be used to treat many different conditions, but our worldwide research group (Cell Surgical Network) has had special interest in its use in treatment for a number of neurologic degenerative conditions.
 SVF has been proven to have immune-modulation properties. In other words, it seems to “re-boot” your immune system and can mitigate autoimmune conditions. There is growing evidence that many of the neurologic conditions that were poorly understood in the past appear to have auto-immune features and the nerve damage is a result of the body’s immune system attacking its own tissues. Parkinson’s disease falls into this category. Some autoimmune conditions like multiple sclerosis (MS) have been long known to be autoimmune. It is still unclear if ALS (Lou Gehrig’s disease) has autoimmune disease features, but there is significant inflammation associated with the ALS nerve damage and SVF is highly anti-inflammatory. Therefore, because of the autoimmune and degenerative nature of so many neurologic diseases, we expect cell therapy to play a role in even the most severe conditions.
SVF has been proven to have immune-modulation properties. In other words, it seems to “re-boot” your immune system and can mitigate autoimmune conditions. There is growing evidence that many of the neurologic conditions that were poorly understood in the past appear to have auto-immune features and the nerve damage is a result of the body’s immune system attacking its own tissues. Parkinson’s disease falls into this category. Some autoimmune conditions like multiple sclerosis (MS) have been long known to be autoimmune. It is still unclear if ALS (Lou Gehrig’s disease) has autoimmune disease features, but there is significant inflammation associated with the ALS nerve damage and SVF is highly anti-inflammatory. Therefore, because of the autoimmune and degenerative nature of so many neurologic diseases, we expect cell therapy to play a role in even the most severe conditions.
Not all neurologic diseases being studied for response to cell therapy affect the central nervous system. Some of the conditions associated with peripheral nerves such as neuropathy and certain chronic pain syndromes including painful bladder syndrome and complex regional pain syndrome (also known as reflex sympathetic dystrophy) are showing evidence that they respond to cell therapy.
One of the most interesting conditions currently being scrutinized by our research group is Alzheimer’s dementia. The project is being led by Dr. Chris Duma, a neurosurgeon at Hoag Hospital in Orange County. Dr. Duma has been working with the team at California Stem Cell Treatment Center using SVF on an investigational basis for advanced neurologic diseases with a special emphasis on MS and dementia. One of the hurdles encountered was finding a way to get high numbers of stem cells into the central nervous system. We all have a bio-barrier separating our blood streams from our central nervous systems known as the “blood-brain-barrier.” This is not a fixed membrane with pores as was originally postulated over 100 years ago but instead a complex and dynamic protective bio-filter that may, in some cases, diminish access of healing stem cells to damaged nerve tissue. One way to bypass the barrier is to inject cells into the spinal fluid which we have done for years, but the most effective and efficient way is to go directly into the ventricles (fluid bathing and surrounding the brain). Dr. Duma and his team have devised a safe way of doing that based on a mechanical device known as the Ommaya reservoir, a system used for many years to introduce chemotherapy into the brain.
Dr. Duma is presenting his SVF data showing safety and clinical improvement in patients with Alzheimer’s and MS at two national neurosurgical congress meetings later this year. Some of the clinical improvement also correlated with positive physical changes as seen in MRIs of the brain.
Stem cells are not effective for all neurologic disease, but we continue to find new uses and strategies for mitigating these diseases using cell therapy. Using your own stem cells that have been freed up from the collagen matrix in belly fat gives us access to very large numbers of healthy stem cells that when deployed in areas of tissue damage, can mitigate that damage and accelerate healing. This is the essence of “cell surgery.”
This is a different model than using someone else’s stem cells patented in a lab and then grown and bottled for use as a medication. It may be many years before such laboratory products are commercially available and patients need access to safe cell therapy today. Our cell surgical research group has just submitted for publication the largest series in the world on autologous (your own) stem cell safety and efficacy for neurologic as well as non-neurologic conditions. It is no longer science fiction. Our patients help fund and participate as part of our investigative work. This is happening today.
Elliot B. Lander, MD, FACS, is co-founder and medical director of The Cell Surgical Network®and Medical Director of the California Stem Cell Treatment Center in Rancho Mirage and Beverly Hills. He can be reached at (800) 231.0407. For more information on stem cells visit www.stemcellrevolution.com






























Comments (0)