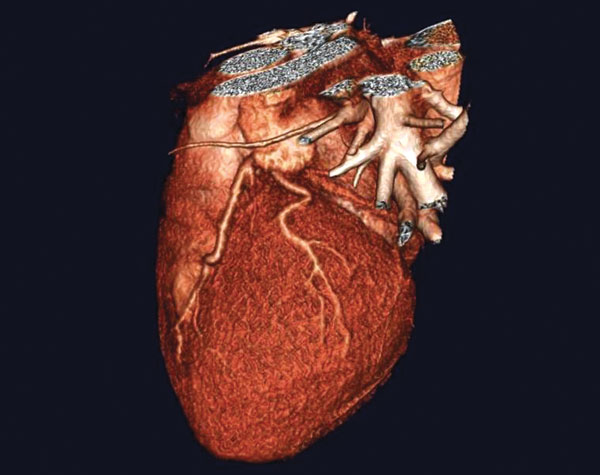
Numerous studies in recent years reveal a strong correlation between obstructive sleep apnea (OSA), where breathing stops while you are sleeping, and atrial fibrillation or “A-Fib”, a leading cause of stroke (see “A-Fib” page 3).
Two primary conclusions of these studies are:
- Those with obstructive sleep apnea are at greater risk of atrial fibrillation1,2
- A-Fib patients with untreated sleep apnea are more likely to revert back into A-Fib after treatment than A-Fib patients without sleep apnea1,2,3
What these findings suggest is that a lack of oxygen while sleeping, commonly recognized by snoring, restless sleep, or fatigue upon waking, can seriously damage the heart, causing irregular heart beat and possibly stroke.
According to StopAfib.org, a site from the American Foundation for Women’s Health, approximately half of A-Fib patients also have OSA. There is a stronger correlation between A-Fib and OSA than any other risk factors.4
Although research hasn’t confirmed OSA as a cause of A-Fib,4 studies show that A-Fib recurrence is higher following two common treatments: electrical cardioversion1,2 and ablation therapy3 in those whose sleep apnea has not been treated. This research also suggests that the longer one has OSA, the less likely ablation is to be successful;3 however, when sleep apnea is treated, A-Fib improves.
How is sleep apnea treated?
Sleep apnea is best treated by a knowledgeable sleep specialist. The goal of treatment is to maintain an open airway during sleep. The challenge for the clinician and the patient is to select an effective therapy that is appropriate for the patient’s problem and that is acceptable for long term use.
Adjust sleep position—Adjusting sleep position (to stay off the back) may help improve sleep quality in people who have OSA when sleeping on the back. However, this is difficult to maintain throughout the night and is rarely an adequate solution.5
Continuous positive airway pressure (CPAP)—A CPAP device uses an air-tight attachment to the nose, typically a mask, connected to a tube and a blower which generates a constant pressure of oxygen. Devices that fit into the nasal opening, rather than over the nose, are also available. CPAP should be used any time the person sleeps (day or night). While the treatment may seem uncomfortable, noisy, or bulky at first, most people accept the treatment after experiencing better sleep. However, difficulty with mask comfort and nasal congestion prevent up to 50 percent of people from using the treatment on a regular basis.5
Nasal valves—Valves that retard expiratory flow can be inserted into each nostril during sleep. This raises the air pressure in the throat and may decrease airway narrowing. The treatment is attractive for travel and camping, and for patients who are unable to tolerate CPAP. However, some patients find the treatment uncomfortable and success is limited in others. Nasal valves are best used for mild cases of OSA when relief of snoring is the main goal.6
Dental devices—A dental device, called an oral appliance or mandibular advancement device, can reposition the jaw (mandible), bringing the tongue and soft palate forward as well. This has been shown to relieve obstruction in some people. Many patients prefer a dental device to CPAP, and therefore compliance is significantly better. Side effects of dental devices are generally minor, but may include changes to the bite with prolonged use.7
Dr. Leonard Feld, DDS, member of the American Academy of Sleep Medicine and sleep apnea specialist states that, “The first step in treatment is to conduct an ambulatory sleep study with a small, take home device which measures important factors like sleep position, oxygen intake and heart rate to determine if the OSA is mild to moderate, moderate to severe, or severe. Next we determine the location of the obstruction. If it has to do with the location of their tongue and the position of the jaw, then it is considered a TMJ disorder and an oral appliance is effective in moving the jaw forward into a more receptive position to maximize oxygen intake and flow.”
Upon diagnosis, Feld confers with the patient’s doctor to determine if an appliance is the preferred form of treatment. “The appliance is clinically proven to be very effective for mild to moderate and moderate to severe cases, but less effective in severe cases.” If test results skew towards severe, a complete sleep study is often recommended.
Feld adds that studies show if the position of the tongue and jaw appear to be contributing factors, oxygen intake may be affected throughout the day as well. “We call it positional adaptation, and what we find with patients who have the appliance (which is worn at all times) is that oxygen intake increases 24/7, improving many aspects of their health.” This would include oxygen to the heart.
“The biggest asset with the appliance is that is treats the cause and opens the airway, whereas the CPAP forces oxygen through the obstructed airway. The oral appliance is also comfortable and easy to wear, so compliance is significantly greater than with CPAP.”
The correlation between A-Fib and sleep apnea is at the forefront of A-Fib research.4 Considering findings to date, it is recommended that if you have OSA, treat it before it possibly leads to a more serious condition. And if you have A-Fib and sleep apnea, be sure to address both conditions with your health care team to maximize treatment results.
For more information on A-Fib, see page 3 of this issue. For more information on sleep apnea, contact Dr. Leonard Feld at the Indian Wells Smile Center. Dr. Feld is the co-founder of the TMJ & Sleep Medicine Network and his philosophy is always conservative, non-invasive and non-surgical treatment. He can be reached at (760) 341-2873. www.DocFeld.com
References: 1) Kanagala, Ravi, MD, et al, “Obstructive Sleep Apnea and the Recurrence of Atrial Fibrillation” http://www.circ.ahajournals.org/cgi/content/full/107/20/2589, Circulation: 2003;107:2589; 2) Gami, Apoor S, MD, et al, “Association of Atrial Fibrillation and Obstructive Sleep Apnea” http://www.circ.ahajournals.org/cgi/content/full/110/4/364, Circulation: 2004;110:364-367; 3) Low efficacy of atrial fibrillation ablation in severe obstructive sleep apnoea patients, Europace, May 20, 2010; 4) Peggy Noonan and Mellanie True Hills “Severe Obstructive Sleep Apnea Predicts Atrial Fibrillation Ablation Failure” July 6, 2010 8:05 AM CT www.stopafib.org; 5) Wolfgang Schmidt-Nowara, MD, Clinical Associate Professor of Medicine, University of Texas Southwestern Wolters Kluwer Health’s UpToDate; http://www.uptodate.com/contents/sleep-apnea-in-adults-beyond-the-basics?source=see_link; 6) Rosenthal L, Massie CA, Dolan DC, et al. A multicenter, prospective study of a novel nasal EPAP device in the treatment of obstructive sleep apnea: efficacy and 30-day adherence. J Clin Sleep Med 2009; 5:532.; 7) Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep 2006; 29:244.































Comments (0)