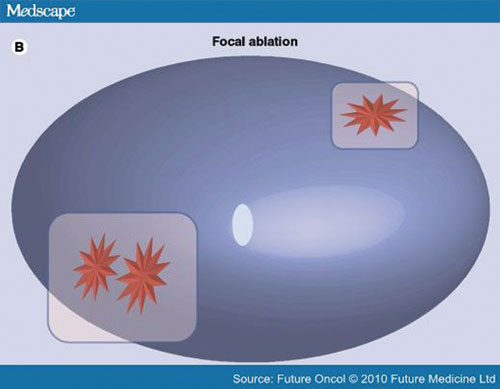
The world of prostate cancer diagnosis has changed significantly over the past thirty years. One of the most notable advances of the past decade is the development of a new biopsy strategy that uses magnetic resonance imaging (MRI). Developed in part by the doctors and scientists at Coachella Valley’s Desert Medical Imaging, the MRI scan helps the doctor identify the areas that look most suspicious. Later those images are used to pinpoint areas for biopsy, unlike conventional systematic biopsy which does not rely on imaging at all. This targeted procedure is less invasive, takes only about 40 minutes and has a high level of accuracy.
For the MRI-guided biopsy procedure, the patient lies face-down inside the MRI scanner. A small needle-guide is placed gently into the rectum. The device is used to get the biopsy needle in the proper place and acts as a fiducial marker. Specialized software allows for precise targeting of the area(s) of interest. Technologist and radiologist work together to obtain the images and collect the biopsy specimens.
Once the biopsy specimens are obtained, they are sent via urgent courier transport to a pathology lab where expert pathologists specially trained in prostate pathology view the tissue under a microscope and assign a Gleason score. The most dominant cell pattern is considered the primary Gleason grade; the second most dominant cell pattern is the secondary Gleason grade. The sum of those two numbers is the Gleason score. The International Society of Urogenital Pathologists (ISUP) has put these scores into categories: ISUP grade one (Gleason score 3+3= 6), ISUP Grade 2 (Gleason score 3+4=7), ISUP Grade 3 (Gleason score 4+3=7), ISUP Grade 4 (Gleason score 4+4=8) and ISUP Grade 5 (Gleason score 4+5 and higher).
Grades 4 and 5 are considered to have the most aggressive potential. To get a window into the future about grades one, two and three, we use genomic testing to evaluate risk further. The beauty of tissue-based genomics is that the information obtained is based on targeted biopsy specimens, so the most meaningful tissue is used.
Desert Medical Imaging has been performing tissue-based genomics for prostate cancer since June 2015. Another advancement in prostate diagnosis was the February 2016 release of a 22-gene panel that provides high, intermediate and low risk categories for biopsy specimens collected using MRI targeting. The additional information provided by the 22-gene panel can help with prognosis and clinical management as it adds another piece to the puzzle and goes beyond just Gleason score alone. The genomic information may also be helpful to solve the issue of disparity among African American prostate cancer patients. Our database of information continues to grow as does our knowledge of this disease.
Bernadette M. Greenwood is Chief Research Officer at Desert Medical Imaging and Clinical Instructor at UC Riverside School of Medicine. For more information about MRI-guided biopsy and tissue-based genomics, contact Desert Medical Imaging at (760) 776.8989 or visit www.DesertMedicalImaging.com.



























Comments (0)