Making a decision to be screened for certain medical conditions can be difficult, especially when the recommendations and guidelines are constantly changing. September is Prostate Cancer Awareness Month and October is Breast Cancer Awareness Month, so it is timely to review the recommendations of various organizations for both of these conditions.
What is a screening test anyway?
Let’s first define the word “screening” as it is used in preventive care. A screening test is a diagnostic test performed on asymptomatic, apparently healthy, individuals in a population. Screening tests help to identify people with increased risk for a condition or disease before they have symptoms or even recognize that they are at risk so that preventive measures can be taken.
Screening tests are an important part of preventive health care. According to the Centers for Disease Control and Prevention, cancer screening tests check your body for cancer before you have symptoms.1 Undergoing screening tests regularly may find some cancers early, when treatment is likely to be most effective.

Breast cancer screening
Breast cancer screening recommendations from the American Cancer Society are age-based, as follows:2 from age 20, women should perform breast self-exam (BSE) and report any new symptoms to their health care professional. From age 20-39, a clinical breast exam (CBE) should be part of a periodic health exam, preferably every three years. After age 40, a CBE and mammogram should be performed annually.
The American Cancer Society also recommends that women at high risk based on certain factors should get an MRI and a mammogram every year. The term “high risk” includes women with about a 20% or greater risk using risk assessment tools based mainly on family history, women who had radiation therapy to the chest when they were between the ages of 10 and 30 years, and women who either have or who are at high risk for mutations in certain genes that greatly increase their breast cancer risk (BRCA1/BRCA2).
Other women who may benefit from screening with breast MRI according to the American College of Radiology include those with newly diagnosed breast malignancy and those with breast augmentation.3 The US Preventative Services Task Force (USPSTF) recommends screening mammography for women, with or without clinical breast examination, every 1 to 2 years for those 40 years and older.4
The USPSTF also recommends that primary care providers screen women who have family members with breast, ovarian, tubal, or peritoneal cancer with one of several screening tools designed to identify a family history that may be associated with an increased risk for potentially harmful mutations in breast cancer susceptibility genes (BRCA1 or BRCA2). Women with positive screening results should receive genetic counseling and, if indicated after counseling, BRCA testing.
Research has recently suggested that men with BRCA2 gene mutation may be at elevated risk for prostate cancer.5

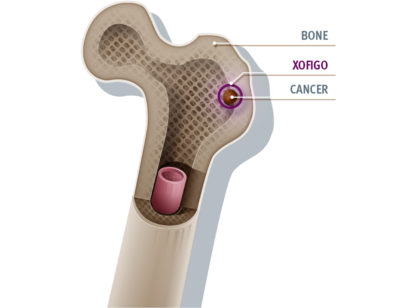
Prostate cancer screening
Prostate-specific antigen (PSA) and digital rectal examination (DRE) have long been the screening tools relied upon for early detection of prostate cancer, confirmed by trans-rectal ultrasound-guided (TRUS) biopsy.
However, according to the American Urological Association, any benefit from use of DRE, derivatives of the PSA test (PSA density, PSA kinetics, and age-adjusted PSA) or molecular forms of PSA (proPSA, freePSA and comlexed PSA) are absent.6 Similarly, the evidence of benefit from urinary biomarkers (PSA3) or imaging (mp-MRI) as first line screening tools has not been documented. Men who have elevated PSA may benefit from the use of DRE and a combination of other tests to determine if a biopsy is necessary or if a cancer was missed at previous biopsy.
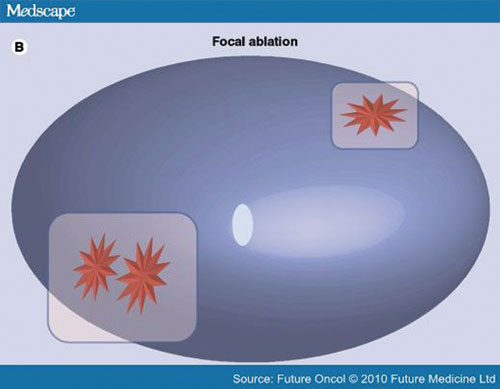
As technology emerges, MR imaging may play a more significant role in the diagnostic workup of screened patients with rising PSA and negative TRUS biopsy. The goal of ongoing research is to identify tumor-suspicious regions within the prostate gland that are not detected during ultrasound-guided biopsy. Targeted biopsies can then be taken improving cancer yield over random, systematic biopsy. MRI may also have an important role in therapy delivery and follow-up.
For men younger than age 55 years and at higher risk (e.g. positive family history or African American race), decisions regarding prostate cancer screening should be individualized. The greatest benefit of screening appears to be in men ages 55 to 69 years.7
The National Comprehensive Cancer Network Guidelines 2014 clearly state that decisions regarding screening for prostate cancer can be very complex for all parties involved: patients, family members and physicians. There are many factors to consider including but not limited to clinical presentation, family history, race/ethnicity, age, and life expectancy.8 Patients must also consider the risks and benefits that detection of prostate cancer carries, and the risks and benefits of treating it.
Some of the risks and potential harms of screening for prostate cancer include a false positive PSA test, over diagnosis, blood in urine or semen from TRUS biopsy, and hospitalization following TRUS biopsy.
If you have questions about whether or not you should undergo screening for any medical condition, speak to your physician.
Dr. Feller is a Board Certified Radiologist at Desert Medical Imaging which offers individualized imaging plans that may include screening, diagnosis, therapy delivery under image-guidance, and follow up. Bernadette Greenwood, Director of Clinical Services at Desert Medical Imaging, is also an author and educator on the topics of breast and prostate MRI. Please visit www.desertmedicalimaging.com for more information or call (760) 694.9559.
REFERENCES: 1. http://www.cdc.gov/cancer/dcpc/prevention/screening.htm. Accessed Aug. 11, 2014. 2. http://www.cancer.org/healthy/findcancerearly/cancerscreeningguidelines/chronological-history-of-acs-recommendations. Accessed Aug. 12, 2014. 3. http://www.acr.org/~/media/2a0eb28eb59041e2825179afb72ef624.pdf 4. USPSTF A and B Recommendations. U.S. Preventive Services Task Force. http://www.uspreventiveservicestaskforce.org/uspstf/uspsabrecs.htm. Accessed Aug. 2, 2014. 5. Kirchoff T et al. BRCA mutations and risk of prostate cancer in Ashkenazi Jews. Clin Cancer Res. 2004 May 1;10(9):2918-21. 6. Turkbey B, Pinto PA, Mani H, et al. Prostate cancer: value of multiparametric MR imaging at 3T for detection–histopathologic correlation. Radiology. 2010; 255:89. 7. Carter HB et al. Guidelines for Early Detection of Prostate Cancer: American Urological Association. 2013. 8. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Early Detection of Prostate Cancer. http://www.tri-kobe.org/nccn/guideline/urological/english/prostate_detection.pdf. Accessed Aug. 11, 2014.




























Comments (0)