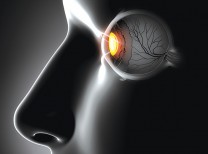
Age-related macular degeneration (AMD) is a condition that can lead to the loss of central vision. For a long time, a patient that progressed to the more advanced “wet” form of the disease was inevitably going to lose the central vision in the eye. Prior to 2005, retina specialists would use laser to destroy the abnormal blood vessels that had grown into the nerve tissue layers. This treatment was effective at destroying the abnormal blood vessels, but it unfortunately also destroyed the overlying retinal tissue leaving patients with significant, often central, blind spots.
In 2005, the first reported cases of the use of a successful medication in the treatment of wet AMD changed everything. The medication was an antibody. An antibody is a protein molecule produced by the body to fight disease. The protein is designed to attach to a bacteria, virus or specific site on a cell. In the case of wet AMD, the antibody was anti-vascular endothelial growth factor (anti-VEGF). What scientists had discovered was that in eyes with wet AMD, there was a protein being produced in the eye that stimulated new blood vessel growth. This protein is not found in a healthy eye. In 2004, an antibody to this protein was developed in the lab as a treatment for colon cancer. The therapy works in cancer by blocking the growth of the blood vessels needed for the growth of a tumor. The discovery that this same antibody could stop the growth of abnormal blood vessels in the eyes of animals, not with cancer but instead with wet AMD, was encouraging. The medication was tried in humans and was very successful in halting the progression of wet AMD and restoring vision. The medications that are currently available as anti-VEGF therapies for the eye are Avastin, Lucentis and Eylea.
For wet AMD, the antibodies have to be delivered directly into the eye. Once inside the eye, the antibodies circulate around and search for any molecules of the vascular growth factor that are being produced by the disease. When located, the antibodies attach to the vascular growth factor making it a much larger molecule. In order for the protein to stimulate the growth of new blood vessels, it must attach itself to the blood vessel wall. I explain to patients that this is like attaching to a docking station. When the antibody-protein complex tries to dock, it can no longer fit because it is too large. So, even though the vascular growth factor is in the eye, it is unrecognizable to the blood vessels since it can’t attach. Without this growth factor, the newly growing blood vessels die. I liken this to turning off the water to newly sprouting plants. The result is rapid withering and death. This process allows your doctor to damage only the unwanted, abnormally growing blood vessels while leaving the healthy blood vessels and retinal tissue undamaged.
As a result of this remarkable treatment strategy, patients with wet macular degeneration can now look forward to a future without vision loss.
Dr. Harrison is a vitreoretinal specialist with Coachella Valley Retina in Rancho Mirage and can be reached at (760) 895.1993.





























Comments (0)