Osteoporosis literally means “ porous bones”. It is a systemic skeletal disease characterized by low bone mass and density, which makes the bones weaker and more prone to fracture. As bones become weak, they can break from minor everyday events such as sneezing or bumping into furniture. One out of every two women and one out of every four men over the age of 50 will experience an osteoporosis related fracture in their lifetime.
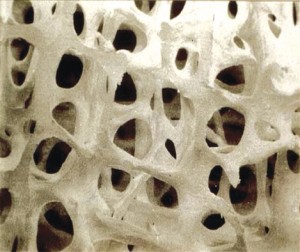
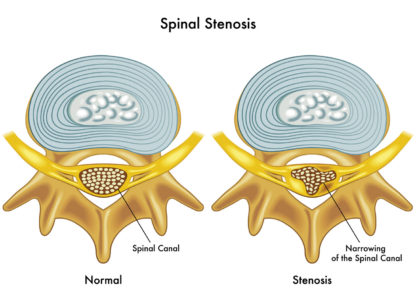
Normal bone
Looking at healthy bone tissue under a microscope, you can see a tight network of fibers. This network is the scaffolding that provides structural strength. In osteoporosis, there are gaps in the scaffolding that represent a loss of bone density and a corresponding loss of strength. This loss in bone density occurs without symptoms, making osteoporosis a silent disease until a fracture occurs.
Osteoporosis is a serious national health problem currently affecting 10 million Americans, and while 8 million of these are women, 2 million are men. Because patients–and the media–tend to worry most about cancer and heart disease, osteoporosis and its effects are often under-reported. Here are some revealing facts about hip fractures:
- Women are 2-3 times more likely than men to experience a hip fracture
- One-year mortality is twice as high for men as for women
- 20% of patients die within one year of a hip fracture
- 30% of patients experience permanent disability; 40% are unable to walk independently post-fracture; and 80% are unable to carry out at least one independent activity of daily living
- Women who have a hip fracture are 4xs as likely to have another one
- A woman’s risk of hip fracture is equal to her risk of breast, uterine and ovarian cancer, combined
Building and maintaining healthy bones is our best defensive strategy. The majority of our adult bone mass (85-90%) is acquired by the age of 18 in girls and 20 in boys. Here are some recommendations from the National Osteoporosis Foundation of things we can do to protect our bones:
- Get enough calcium and Vitamin D every day. It is recommended that women get 1000 mg of Calcium and at least 400 – 800 IU of Vitamin D if they are under age 50, and 1200 mg of Calcium with 400 – 800 IU of Vitamin D over age 50. It is recommended that men get 1000 mg of Calcium with 800 IU of Vitamin D up to age 70, and 1200 mg of calcium with 1000 IU of Vitamin D age 70 and over. For both men and women, your doctor may recommend more Vitamin D as appropriate.
- Get regular weight bearing and muscle building exercise. Weight bearing exercises make you move against gravity. Examples include: dancing, aerobics, hiking, jogging or running. Low impact examples are elliptical trainers, stair-step machines or walking on a treadmill or outside.
- Don’t smoke and limit alcohol intake. Smoking negatively affects bone by damaging blood vessels and reducing the amount of available oxygen. It also causes an increase in cortisol. Cortisol increases bone breakdown. In addition, smoking releases free radicals, which damage the cells that build new bone. Excessive alcohol inhibits the actions of bone building cells and may also impair balance, thereby increasing the risk of falls.
- Talk to your doctor about your risk of osteoporosis and a bone density test. Your doctor can review your personal and family history to assess your risk for bone loss. A Dual-energy X-ray Absorptiometry, or DXA, is the gold standard for diagnosing low bone density and predicting fracture risk. In the absence of risk factors women should start screening at age 65 and men at age 70. Your doctor may recommend screening earlier if you have risk factors. The DXA gives you a T score. This score, along with your age and other risk factors, is used to assess your risk for fracture.
- Take a bone building medication if right for you. If your fracture risk assessment is high, your doctor will likely recommend treatment. There are many factors to consider and many different medications. Calcitonin and hormonal therapies (Estrogen, Evista and Prolia) are only approved for women. The Bisphosphonates (Fosamax, Actonel, Boniva, Reclast, Zometa) and Forteo are approved for both men and women. Other factors are age, menopausal status, medical conditions, and severity of bone loss. The Bisphosphonates have come under scrutiny recently with information on atypical femur fractures. Many experts now recommend stopping these medications after 3-5 years of therapy. It may be restarted after a 2-3 year drug holiday, or a different medication may be selected.
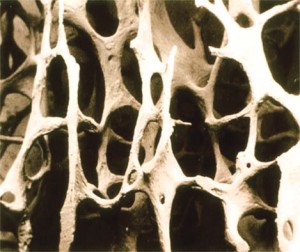
Osteoporotic bone
Risk factors for osteoporosis. Major risks are age greater than 70, early menopause (younger than 45 for women), prior fracture, steroid use, and low body weight.
No medication is risk free. The goal is to balance informed risk vs. proven benefit for each individual patient.
Dr. Lindley is a board certified Gynecologist. She has been practicing since 2002 on the Eisenhower campus and is currently part of Eisenhower’s E365 program, providing gynecology and primary care for women. For information call 760- 837-3999.
Resources: 1) Davis, JL, The Effects of Smoking on Bone Health, WebMD, 2005, June 2012, http://www.webmd.com 2) Nat’l Osteoporosis Foundation, NOF, June 2012, http://www.nof.org; 3) Osteoporosis, The Free Dictionary, Farlex, Inc., June 2012, http://www.medical-dictionary.thefreedictionary.com 4) Sampson, HW, Alcohol and Other Factors Affecting Osteoporosis Risk in Women, Nat’l Institute for Alcohol Abuse and Alcoholism, NIH, USA.gov, 2003, June 2012, http://www.pubs.niaaa.nih.gov
























Comments (2)
Why isn’t strontium renolate approved in this country. It is widely used throughout Europe ,
Hi Ellen, That’s a great question. There are several reasons that it has not been approved in
this country. Here is an excerpt from BoneHealth Blog that you might find helpful….
“Strontium ranelate is available by prescription under various names in some 70 countries for the treatment of post-menopausal osteoporosis. When taken by mouth at up to 2 mg per day on average strontium renelate shows improved bone strength and reduced fracture rates in women with osteoporosis.
But the risks of taking strontium ranelate can be serious – increased risk of blood clots and memory loss have been reported. Strontium is also known to accumulate and remain in the body for long periods of time. For these reasons the United States Food and Drug Administration (FDA) has not approved the use of strontium ranelate for U.S. consumers.”
There is also an article in Medscape discussing the recommendations by the EU in April 2013 to restrict the use of strontium based on increased risk of serious cardiac events.
The FDA has determined that the benefits of strontium do not outweigh the risks, and the European Medicines Agency confirmed the recommendation to restrict its use in Europe.
I hope this answers your question. Dr. Lindley