Prostate Cancer is the most common cancer in men with 1 in 6 men being diagnosed with the disease at some point in their life. Like any cancer, early detection of prostate cancer gives the patient more options for managing or treating their disease.
Currently, the most widely used screening tools for prostate cancer are the Digital Rectal Exam (DRE) and Prostate Specific Antigen (PSA) blood test. The PSA blood test was approved by the FDA in 1986 for monitoring confirmed cases of prostate cancer, and was approved in 1992 for screening for prostate cancer. Studies have shown that the introduction of screening serum PSA for detecting prostate cancer reduced the number of deaths from prostate cancer by 20%; however, it also has led to an increase in over diagnosis and overtreatment of prostate cancer. Overtreatment of low risk prostate cancer can include unnecessary whole gland therapies such as radical prostatectomy and radiation therapy which have potential long term side effects, mainly erectile dysfunction and urinary incontinence.
Over the past five years clinicians have learned more about the behavior of prostate cancer which has enabled physicians to treat intermediate and high risk cancer while only monitoring low risk cancers that would never kill a patient. Research has determined that patients with low risk prostate cancer (serum PSA< 10 ng/ml, Gleason Score 3+3=6 or less, low volume, confined to the prostate gland) have a very small chance of developing metastatic disease and a very small chance of dying from their prostate cancer. This represents approximately 45% of newly diagnosed prostate cancer patients in the U.S. and Canada, or approximately 150,000 men per year. Monitoring low risk prostate cancer is categorized as Watchful Waiting (WW) and Active Surveillance (AS). These terms have been used interchangeably for years, but there are differences between them.
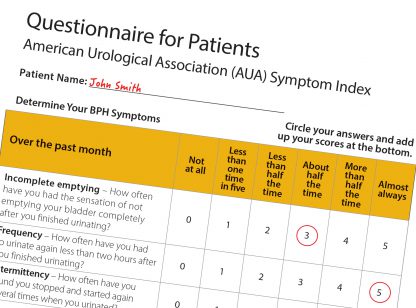
Watchful Waiting (WW) is for men who have low risk cancer and a life expectancy of less than 10 years, or have a history of serious health problems that may make some treatments too risky. Typically, patients will have a DRE and PSA test every 6 – 12 months. Hormone therapy may be used if the cancer begins to spread and the patient becomes symptomatic.
Active Surveillance (AS) is appropriate for younger men with low risk cancer who wish to postpone or avoid definitive treatment, or older men for whom the cancer may never cause a problem. Typically patients will have a DRE and PSA every 3 – 6 months and a biopsy once a year.
Areas of concern for both of these methods are the accuracy of the diagnosis of the cancer. PSA tests can identify if there is a problem, but it can’t distinguish the cause. PSA levels can be elevated due to prostate cancer but also due to benign causes such as BPH (benign prostatic hyperplasia) or prostatitis. The Gleason Score is the most important biomarker for determining the prognosis of prostate cancer. Currently, most pathology scores needed to determine Gleason Scores are acquired through a Transrectal Ultrasound-guided biopsy (TRUS). While TRUS biopsies are still the most common method for biopsy, it has an error rate of 35% because the samples are taken randomly. Random sampling can also find clinically insignificant cancers while missing a more aggressive cancer. Also, some tumors may be under graded (under Gleason Scored) due to the random sample picking up the low grade portion of the tumor and missing the high grade component. This contributes to the fact that over time, one third of patients in Active Surveillance will be reclassified as higher risk for progression of their prostate cancer and will then be offered definitive treatment.
New technology has emerged that will assist physicians in more accurately Gleason Scoring a patient’s cancer before electing to go on watchful waiting or active surveillance of the cancer. Radiologists have developed a diagnostic imaging exam called a Multiparametric MRI of the prostate gland which accurately detects tumor-suspicious regions that can then be targeted with MR guided biopsy of the prostate gland. This type of biopsy is targeted, not random.
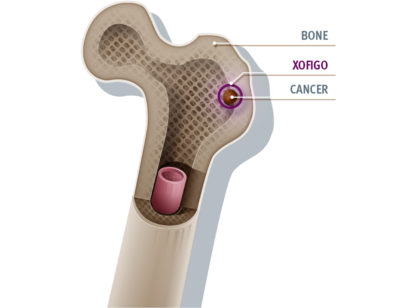
A Multiparametric MRI uses three different types of images to see inside the prostate gland. The first are T1- and T2-weighted imaging which show the anatomy of the gland. Second is diffusion- weighted imaging (DWI) which identifies areas where motion of water molecules is restricted due to cancer tissue, and the third is dynamic contrast enhanced imaging (DCE)which uses gadolinium-based contrast to find areas where new blood vessels are growing (cancer cells make their own blood vessels to supply themselves with oxygen and nutrients). All of these images are sent to a computer workstation to aid the radiologist in interpreting the images with the goal of finding tumor-suspicious regions. This is called Computer Aided Detection (CAD).
Should a tumor-suspicious region be found, a real time MRI-guided biopsy can be performed to acquire core samples from the target region and accurately determine the Gleason Score. MRI-guided biopsies have a 90% accuracy core sampling rate compared to TRUS’s 65% accuracy rate for prostate cancer with a Gleason Score of 7 and above.
Benefits of MRI for assisting in Watchful Waiting and Active Surveillance are:
• Multparametric MRI’s are non-invasive. Patients who elect WW or AS can get a baseline study performed to make sure they are truly a good candidate for expectant management. While in AS or WW, the Multiparametric MRI can be repeated if there is a change in the DRE or PSA to determine if there is a higher risk of progression of the prostate cancer.
• MRI-guided biopsies can ensure that the Gleason Score is accurate so that patients may be correctly directed to WW/AS or definitive treatment.
If you or a man you know is considering conservative management of prostate cancer, the good news is that there is an important emerging role for MRI. Multiparametric MRI is proven to be helpful in the detection and localization of prostate cancer as well as helping to determine the prognosis and appropriate management of patients with prostate cancer.
Dr. Feller is a Board Certified Radiologist at Desert Medical Imaging which has a MRI based prostate cancer program. Please visit their website www.desertmedicalimaging.com for more information or call 760.694.9559.




























Comments (0)